Spontaneous Aortic Thrombosis i6 (PDF)
File information
This PDF 1.4 document has been generated by Online2PDF.com, and has been sent on pdf-archive.com on 24/08/2017 at 07:52, from IP address 117.223.x.x.
The current document download page has been viewed 312 times.
File size: 113.39 KB (8 pages).
Privacy: public file


File preview
Spontaneous Aortic Thrombosis i6 a
Neonate Presenting as Coarctation
By Dr. PATRICIA ANN PENKOSKE, M.D.
ABSTRACT Spontaneous aortic thrombosis in the
neonate is a rare entity of uncertain etiology with a
high mortality. To our knowledge, this is the first
report of a newborn surviving surgical treatment of
spontaneous thrombosis of the thoracic aorta.
Aortic thrombosis in neonates is rare and usually
related to umbilical artery catheterization.
Spontaneous aortic thrombosis in a neonate has
been described [14]. The location is more commonly
abdominal than thoracic. Management has been
varied and usually unsuccessful. Spontaneous
thrombosis of the thoracic aorta has been lethal in
the cases reported [4, 51. We report the case of a
newborn with spontaneous thrombosis of the
thoracic aorta who was treated surgically and
survived.
This 2,810-gm, 38-week-gestation male infant was born
to a 33-year-old gravida I1 para I mother. Prenatal
history was normal until the day of delivery when
she was seen with absent fetal movements.
Emergency cesarean section was performed. The
infant had marked respiratory depression, with Apgar
scores of 4 and 8, and required resuscitation.
The skin appeared mottled but pink. Heart rate was
130 beats min, respiratory rate was 64/min, and
blood pressures were: 106194 mm Hg in the right
arm, 84/66 mm Hg in the left arm, 36/25 mm Hg in
the right leg, and 48/31 mm Hg in the left leg.
Precordial impulse was increased, and the liver edge
was 3 cm below the right costal margin. The left
femoral pulse was palpable but decreased. The right
femoral pulse was not palpable. A Grade 216 systolic
ejection murmur was audible at the heart base.
Umbilical arterial catheterization had not been
performed. Arterial blood gases were pH 7.27,
carbon dioxide tension was 48.5 mm Hg, oxygen
tension was 37 mm Hg, and hematocrit was 66.5%.
Chest radiograph showed moderate cardiomegaly
and mild pulmonary plethora.
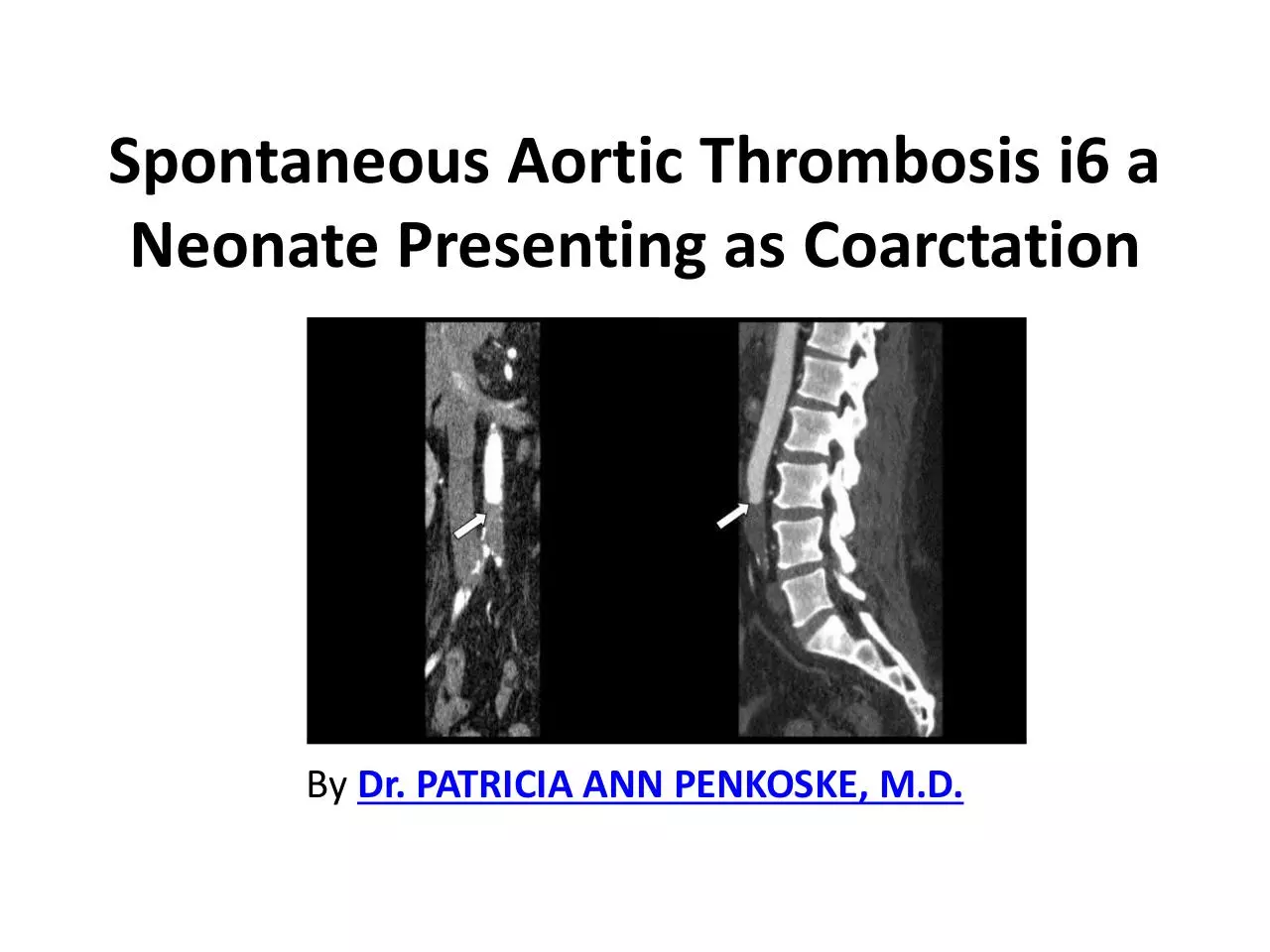
Two-dimensional echocardiography demonstrated a
structurally normal heart but the almost complete
narrowing of the aorta just above the level of a persistent
ductus arteriosus. Left ventricular contractility was
markedly reduced, with a shortening fraction of 0.13
(normal, 0.2tL0.50). An infusion of prostaglandin El, 0.05
mg/kg/min was started. Cardiac catheterization was
performed. Left ventricular pressure was 86/12 mm Hg,
and the descending aortic pressure was 32/26 mm Hg.
Figure 1 shows the posteroanterior view of the aortic
arch from the left ventricular angiogram. There was the
obstruction in the right subclavian artery at the level of
its exit from the thorax and a severe stenosis of the left
the subclavian artery with a thrombus within this vessel.
The lateral view (Fig 2) demonstrated an obstruction to
flow distal to the left subclavian artery.
In the operating room, the aortic arch was visualized
through a left-sided thoracotomy. The aorta was
opened and an organized, partially adherent
thrombus was removed. The thrombus originated
just distal to the left carotid artery and sent a tail into
the left subclavian artery, which was hypoplastic. The
ductus arteriosus was patent, with no thrombus in its
lumen. There was no visible external coarctation or
posterior shelf internally. The aorta was closed with a
Gore-Tex patch to prevent narrowing from surgical
scamng at the incision line. Pathological study
demonstrated a clot measuring 6 x 5 x 4 mm that
consisted of fibrin and foci of calcification.
The platelet count fell gradually to 34,000/~1 on the fourth
postoperative day but then returned to normal.
Prothrombin time was 13.1 to 13.5 seconds (normal,
1S30 seconds). Partial thromboplastin time was 45
seconds on the second postoperative day (normal, = 4665 seconds). Protein C and antithrombin I11 levels were
below normal: protein C was 0.45 units (normal, 0.631.27 units) and antithrombin I11 was 0.47 units (normal,
0.75-1.25 units).
Postoperatively, the left femoral pulse was normal. Signs of
congestive heart failure resolved quickly. The right
femoral pulse did not return, and an ischemic area
developed on the tip of the right small toe. The rest of
the limb was pink and well perfused. The right arm was
intermittently cyanosed, and the pulse was absent. Heart
size returned to normal by the fifth postoperative day.
The infant has been followed up for six months and is
developing normally and is receiving no medications.
Contact Us:
Dr. Patricia Penkoske
About us: Dr. Patricia Penkoske is experienced
Cardiothoracic Surgeon and thoracic surgery doctor
in Saint Louis, Missouri.
Address:4944 Lindell Blvd, 4 West, St. Louis, Mo. 63108
General Inquiries: patricia.penkoske@gmail.com
Phone: 314-753-5255
Citizenship: USA, Landed Immigrant-Canada.
Download Spontaneous Aortic Thrombosis i6
Spontaneous Aortic Thrombosis i6.pdf (PDF, 113.39 KB)
Download PDF
Share this file on social networks
Link to this page
Permanent link
Use the permanent link to the download page to share your document on Facebook, Twitter, LinkedIn, or directly with a contact by e-Mail, Messenger, Whatsapp, Line..
Short link
Use the short link to share your document on Twitter or by text message (SMS)
HTML Code
Copy the following HTML code to share your document on a Website or Blog
QR Code to this page
This file has been shared publicly by a user of PDF Archive.
Document ID: 0000658986.